
6 Ways to Reduce Medical Errors in Hospitals and Save Lives
Medical errors remain a serious threat to patient safety. But evidence shows that many medical errors are preventable through systemic changes and best practices.
In U.S. hospitals alone, an estimated 1.2 million patients are harmed each year by medical errors. At Lumeto, we’ve experienced firsthand how the right training can reduce medical errors.
In this article, we will walk through six proven strategies that can reduce unnecessary medical errors without overwhelming your team.
Types of Medical Errors and Their Consequences
Medical errors can occur at many points in care. Here are common types of errors and their impact on patients and providers.
Diagnostic Errors
The National Academy of Medicine defines diagnostic error as “the failure to establish an accurate and timely explanation of the patient’s health problem or to communicate that explanation.”
These failures often occur not because of a lack of knowledge, but because of system breakdowns. Common causes include:
- Incomplete patient histories or rushed exams
- Insufficient diagnostic training
- Communication gaps between care teams
- Cognitive biases like anchoring or premature closure
- Inadequate access to diagnostic tools or follow-up
40,000–80,000 deaths in the U.S. each year are attributed to diagnostic errors, according to the Joint Commission. Approximately 10% of U.S. patient deaths are thought to involve diagnostic error.
Medication Errors
Medication errors happen when there’s a mistake in prescribing, dispensing, dosing, or administering drugs. These can lead to untreated illness, allergic reactions, drug toxicity, or even death. Globally, the World Health Organization estimates that medication errors cost $42 billion each year.
For example, a nurse might accidentally administer hydroxyzine instead of hydralazine, resulting in organ damage or a complete lack of blood pressure control.
In the U.S., efforts like Computerized Provider Order Entry (CPOE) systems have helped. Many hospitals have adopted CPOE, with some ICUs seeing up to an 85% reduction in prescribing errors after switching from paper-based orders.
As a VR training platform built specifically for healthcare, Lumeto enables healthcare staff to get ready for real-world medication administration. Trainees can handle high-risk drugs and learn to avoid mix-ups in emergencies.
Here’s a video of a trainee practicing drug administration in a simulated hospital scenario:
Communication Errors Between Care Teams
When doctors, nurses, pharmacists, or other team members fail to share critical information or miscommunicate, patients can suffer. According to a U.S. study, communication failures were linked to 1,744 patient deaths over five years.
Common communication errors include:
- Handoff miscommunications
- Unclear responsibilities
- Omitted information
- Ambiguous instructions
- Breakdowns across departments
Documentation and Data Entry Mistakes
Even with the widespread adoption of Electronic Health Records (EHRs), documentation errors continue to put patients at risk. Sometimes, in new ways, such as:
- Selecting the wrong patient chart
- Autopopulated fields carrying over incorrect data
- Illegible handwriting or transcription errors
- Incomplete documentation
- Data entered under the wrong section or provider
One study reviewing electronic charts of cancer patients found that 15% contained documentation errors related to diagnosis or treatment—errors that could delay or derail care.
Surgical Errors
Surgical errors may be less common than other types of medical mistakes, but their consequences are often severe. According to the World Health Organization, over 1 million patients die each year from surgical complications worldwide.
Even when not fatal, these errors can lead to:
- Unnecessary repeat surgeries
- Longer hospital stays and recovery times
- Permanent disability or disfigurement
- Emotional and financial distress for patients and families
One of the most effective interventions has been the use of a surgical safety checklist. Human factors training, including teamwork, decision-making, and situational awareness, has also been shown to reduce surgical errors.
How to Reduce Medical Errors with Evidence-Based Practices
Here, we outline some proven strategies to reduce medical errors:
Train Clinical Decision-Making Under Pressure
Healthcare providers often face critical moments where fast, accurate decisions mean the difference between life and death. One such example is responding to a cardiac arrest. In such a scenario, trainees manage a sudden drop in vitals or deal with unexpected complications in surgery.
Simulation-based training helps prepare clinicians for these high-stakes situations. Instead of only reading protocols or observing procedures, staff learn by doing. They practice in realistic scenarios where they can safely make mistakes and receive immediate feedback.
One of the most effective components of simulation training is debriefing. After the scenario ends, learners reflect on what went right and what broke down.
On Lumeto’s InvolveXR, both trainers and trainees can review detailed performance reports to pinpoint what went well and what needs work.
Here’s an example:

This is where the “pressure learning” is consolidated. People can realize “I missed that clue because I got tunnel vision” and think about how to avoid that next time.
At Lumeto, we’ve designed immersive VR simulations that replicate these clinical moments with precision.
Reduce Cognitive Overload
Cognitive overload and fatigue are major contributors to medical errors. The Institute of Medicine has compared working after 24+ hours without sleep to being legally intoxicated.
In hospitals, it shows up like this: A nurse is preparing medications, gets interrupted by an alarm or a question, and returns to the task, unsure if they already scanned the vial or double-checked the dosage.
Technology can help reduce this burden. Tools like automated medication dispensing systems, clinical reminders, and digital handoff checklists are designed to support memory and reduce error. But when poorly designed, these tools can add to the problem (flooding staff with constant alerts and notifications).
VR training reduces cognitive overload by allowing staff to build mental models before entering high-stakes situations.
In VR, providers can:
- Practice clinical routines until they become second nature
- Learn how to respond under pressure without real-world distractions
- Strengthen muscle memory and decision-making pathways
- Experience realistic interruptions and learn how to manage them safely
Expose Staff to Culturally Sensitive Scenarios
Medical errors don’t always stem from clinical gaps—sometimes, they happen because of cultural misunderstandings or communication barriers.
Examples include:
- A provider misinterpreting a patient’s description of pain due to culturally specific idioms
- A language barrier leading to the wrong dosage or misunderstood discharge instructions
- Failing to account for religious or cultural preferences during treatment discussions
Research shows that improving cultural competence in healthcare teams directly supports better communication.
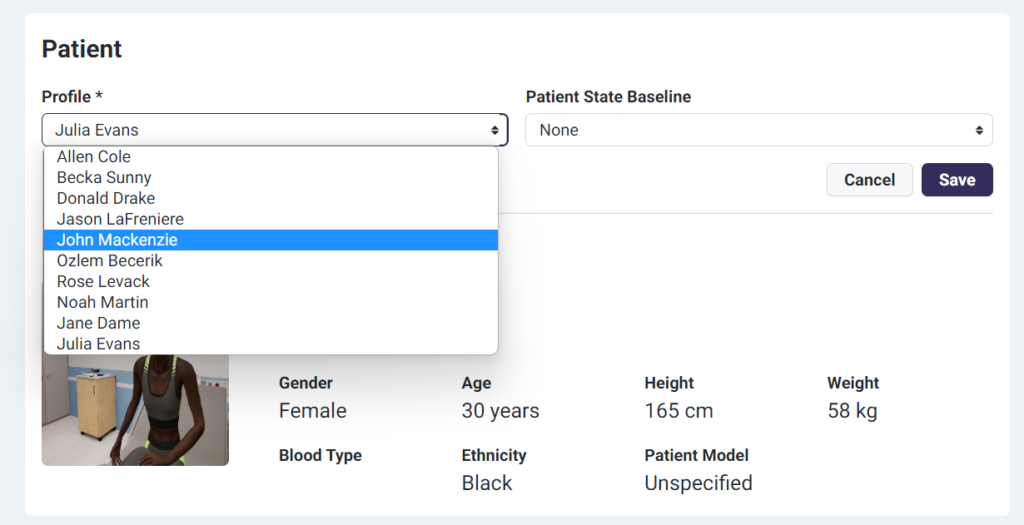
With Lumeto, healthcare teams can train in culturally relevant, emotionally complex simulations. Trainees can interact with virtual patients and practice communicating with clarity and respect, even across language barriers. Trainers can customize the following variables:
- Patient Information and Medical History
- Patient Symptoms & Baselines
- Patient Dialogue & Responses
Here’s a look at how providers can select and design virtual patients for immersive, culturally diverse training:
Improve Competency with Real-Time Feedback
One of the most effective ways to improve clinical skills is through real-time feedback.
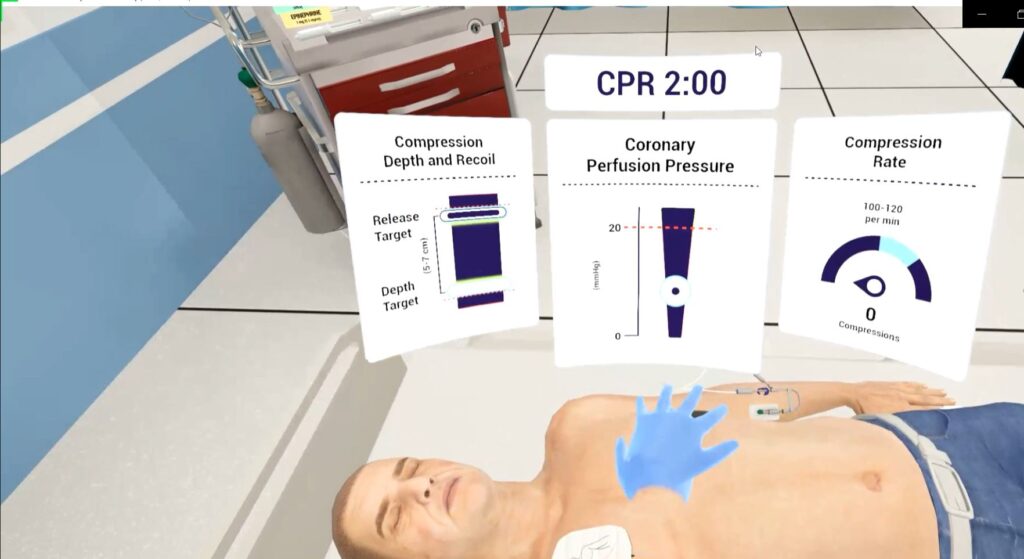
Lumeto’s VR platform delivers this kind of feedback during immersive clinical simulations. For example, during CPR training, learners can see:
- Compression depth and recoil measured in real time
- Compression rate compared to the target
- Coronary perfusion pressure indicators to evaluate CPR effectiveness
The feedback loop builds muscle memory and increases confidence. It is more likely that the correct technique will be applied in real emergencies.
Here’s an example:
Some hospitals have instituted “watcher” programs where an experienced clinician rounds and provides on-the-spot coaching or catches unsafe practices.
Enhance Communication in Team-Based Care
In complex environments like hospitals, even the best clinical judgment can fall apart if team members don’t understand each other clearly.
Structured tools like SBAR (Situation, Background, Assessment, Recommendation) have become widely adopted. They improve how nurses and physicians exchange critical information.
In Lumeto’s ACLS (Advanced Cardiac Life Support) sessions, teams practice this kind of structured, high-stakes communication in a safe, virtual setting. As shown in the video below, trainees work through emergency scenarios together:
Build Empathy
Empathy in practice means truly hearing the patient. For example, an empathetic doctor will take a patient’s worries about a symptom seriously rather than dismissing them. It could make the difference in pursuing an accurate diagnosis versus writing it off.
Consider a scenario: a patient says, “I don’t feel right after that medication.” A busy, harried response might be “It’s fine, just take it.” But an empathetic response would inquire further, possibly uncovering that the patient got the wrong medication or dose.
Programs like The Joint Commission’s “Speak Up” reinforce this principle by encouraging patients to voice their concerns.
In emotionally charged situations, empathy also helps de-escalate tension.
Lumeto has advanced this further by creating the industry’s first conversational AI virtual patient.
Previously, training relied on pre-scripted dialogue. Now, with Lumeto’s platform, trainers can guide interactions in real time:
- Adjust the patient’s tone and emotional response through a live dashboard.
- Practice nuanced conversations that reflect real-world complexity.
“I have been struck by how working with AI patients in Lumeto evokes an emotional response that mirrors interactions with human patients. The joy of making a breakthrough in patient communication or the sadness felt during a patient’s distress highlights the system’s realism and immersiveness. This emotional engagement makes each simulation a powerful tool for honing empathetic and professional skills as a nurse.”
—Kimberly Workum, Director, Clinical Competence Assessment Centre and Digital Strategies Senior Instructor, College of Nursing, Rady Faculty of Health Sciences, University of Manitoba
Challenges in Medical Error Prevention
Healthcare systems face significant challenges in advancing patient safety. Some of them are listed below:
Lack of Access to Modern Technology
Smaller or under-resourced hospitals have limited access to modern technology. Rural facilities often face financial and infrastructure constraints. The adoption of tools is usually delayed or blocked, like EHRs, CPOE, or advanced simulation training.
The same issue holds true for VR-based training systems. Many hospitals see the potential but hesitate due to concerns about cost, technical setup, or the IT resources required to maintain new platforms.
But Lumeto was specifically built to remove those barriers.
You don’t need a simulation center or enterprise-grade IT to get started. Lumeto’s platform works with affordable consumer-grade hardware like the Meta Quest 2 or 3, and a standard PC laptop (no Mac needed).
The setup process is fast and straightforward:
- VR equipment configuration and support provided directly by Lumeto
- Network troubleshooting and consultation included
- Multi-site support available for institutions with multiple campuses
- Average setup time is just 2 hours per location
- Only residential-grade Wi-Fi is required
Shortages in Staff
Research shows that as nurse-to-patient ratios worsen, error rates rise. And the problem isn’t going away. Federal projections estimate a shortage of 78,610 full-time registered nurses (RNs) in the U.S. by 2025.
It requires policy-level solutions, such as:
- Funding for more nurse education programs
- Incentives for rural and underserved area placements
- Improved reimbursement rates to support safe staffing levels
Lumeto’s immersive training has been used to accelerate the onboarding of IENs. It allows them to learn U.S. hospital protocols and emergency response workflows safely. Overseas trainees can learn communication best practices without needing to wait for in-person simulations.
By training IENs in a virtual environment, hospitals can:
- Reduce onboarding time
- Ensure consistent skill-building
- Prepare nurses for local expectations and safety protocols
- Address staff shortages faster without compromising patient care
Underreporting of Errors Due to Fear
Not all medical errors or near-misses are reported, often because staff fear blame and punishment.
Underreporting is problematic because learning from mistakes is central to preventing future ones. Once we have the root cause analysis, only then can systems be redesigned. If fear causes only a fraction of errors to be reported, hospitals operate with an incomplete picture of their safety vulnerabilities.
In a just culture, the focus shifts from blame to accountability and learning. Staff are encouraged to report mistakes without fear, and leadership distinguishes between:
- Blameless errors: such as system flaws or reasonable human mistakes
- Blameworthy errors: like willful neglect or dangerous behavior
When staff see that mistakes are viewed as learning opportunities (not career threats), they’re more likely to report real-world incidents. VR training supports this culture shift by allowing staff to reflect on mistakes in a safe, simulated environment.
Overload from Alert Fatigue
A 2014 study in one hospital’s ICU found over 2 million monitor alarms in a single month. That’s an average of 187 alarms per patient per day. Additionally, in primary care, doctors might receive over 100 electronic alerts per day for things like test results or drug interactions.
Clinicians start to tune out alerts. Studies show that doctors and nurses override or ignore the majority of electronic alerts. A Boston Globe investigation found over 200 deaths in a five-year span linked to ignored alarms from physiologic monitors.
Hospitals are now forming alarm or alert committees to assess which alerts are being ignored and why. It helps in reconfiguring systems to reduce false positives or non-critical alarms.
Lumeto Helps Reduce Medical Errors Through VR Training
Medical error prevention depends on consistent training and system-level readiness. Lumeto’s immersive VR tools help healthcare teams prepare for complex scenarios before they happen in real life.
Hospitals and training institutions now use Lumeto as a core part of their simulation strategy, complementing manikin-based programs with highly flexible, scalable, and accessible VR learning.
“We have integrated Lumeto as a regular recurring station in parallel with our high fidelity manikin program and the feedback from learners has been overwhelmingly positive.”
— Dr. Timothy J. Koboldt, Simulation Director, University of Missouri – Columbia School of Medicine
Lumeto offers over 800 customizable tools for various scenarios and patient types. There are also 200+ interactive medical equipment items across a range of virtual environments (including hospitals, observation rooms, and field tents).
Our Train-the-Trainer program helps institutions confidently launch and scale VR training. In just three 1.5-hour sessions, educators learn how to deploy scenarios, run mock sessions, and reinforce product knowledge using interactive support materials.
FAQs About Prevention of Medical Errors
Which is a medical error prevention strategy hospitals often overlook?
Cultural competency training is often underused. Many medical errors stem from misunderstandings rooted in language barriers or cultural assumptions.
Are certain departments more prone to medical errors?
Yes. High-acuity departments like ICUs, emergency departments, and remote health workers tend to have higher error rates due to time pressure, patient complexity, and volume of alerts.
What role do patients play in reducing unnecessary medical errors?
Patients are a critical part of the safety equation. When they feel comfortable speaking up, asking questions, or reporting concerns, errors can be caught before harm occurs.