
Why Patient Safety Training Fails—And How VR Fixes It
Every year, preventable medical errors contribute to hundreds of thousands of patient deaths in the U.S. alone. Yet, many training programs rely on outdated methods that don’t prepare staff for real-world challenges.
At Lumeto, we’ve seen how immersive, scenario-based patient safety training can better equip teams to act quickly and safely under pressure.
In this article, we’ll explore why patient safety training often falls short and how virtual reality (VR) can make it more effective.
What’s Included in Patient Safety Training?
Patient safety training teaches healthcare workers how to prevent harm during care. According to the World Health Organization, it involves improving knowledge, skills, systems, and behaviors that reduce the risk of avoidable injuries or errors in healthcare settings.
Each year, medical errors contribute to an estimated 250,000 deaths in the United States. That makes them one of the top causes of death. Many of these incidents are preventable with proper preparation and communication.
Preventing Patient Handoff Errors
Patient handoffs (between shifts or departments) are one of the most common points of failure in clinical care. It’s no surprise that around 67% of serious communication breakdowns in hospitals are tied to poor handoffs.
Effective patient safety training includes structured handoff protocols and role clarity. Students learn techniques to communicate clearly every time a patient changes hands.
Reducing Medication Mistakes
Medication errors are a leading cause of preventable harm. In the U.S. alone, they result in one death per day and 1.3 million injuries annually. Globally, these mistakes contribute to 2 million deaths per year and cost healthcare systems about $42 billion.
Patient safety training focuses on improving accuracy in drug administration. It also teaches staff how to stay focused during interruptions.
Improving Infection Control Compliance
According to the CDC, 1 in 31 hospital patients in the U.S. has at least one healthcare-associated infection (HAI) at any given time. Healthcare trainees should learn protocols for hand hygiene, PPE usage, sterile technique, and environmental cleaning.
Fall Prevention and Mobility Assistance
Patient falls are one of the most common safety incidents in hospitals, and they can have life-altering consequences. Each year, an estimated 700,000 to 1 million patients fall while in U.S. hospitals.
A fall in a healthcare facility is so serious that if it leads to major injury, it’s considered a “never event” (completely unacceptable) and not even reimbursed by Medicare. That’s why fall prevention is a critical part of patient safety training for nurses and other medical staff.
Bedside Communication & Empathy
Misunderstandings about care plans, symptoms, or medications can lead to delayed treatment or non-compliance. That’s why patient safety curricula often include modules on communication skills and situational awareness.
Empathy training is also gaining ground as a formal part of safety education. One study found that law enforcement officers who underwent VR-based de-escalation training showed measurable increases in empathy scores.
Lumeto is a medical training platform that has developed first-ever customizable conversational AI in VR. It lets learners interact with virtual patients using real dialogue. Learners can train on scenarios like:
- De-escalating a distressed patient
- Explaining a patient’s condition to the attendant
- Building rapport with someone from a different cultural background
- Clearly communicating discharge instructions
Here’s an example of a medical student working with a virtual patient on Lumeto:
Crisis Response
At one VA hospital, 31% of in-hospital cardiac arrests occurred outside of ICU settings, where immediate intervention can be even more challenging.
Patient safety training prepares staff for these high-stakes scenarios by reviewing protocols and assigning roles during rapid response. The goal is to build muscle memory so staff can respond quickly and confidently, even if they’ve never seen the event before.
Why Traditional Patient Safety Training Programs Fall Short
Although we know what to teach, patient safety training often fails to create a lasting impact. Several key shortcomings have been identified:
Outdated Methods
Many training programs still rely heavily on lectures, slide decks, or simple online modules to cover patient safety topics. The problem is that passive learning yields limited retention. Learners simply don’t remember or internalize much from a PowerPoint or a memo after a few days.
One analysis by PwC found VR-based learners retained 75% of the taught information (versus 5–10% via classroom or e-learning) and were 4 times faster to train.
Limited Exposure to Rare or High-Risk Scenarios
A big challenge in patient safety education is how to train for events that happen infrequently but have critical consequences.
For example, a nurse could go years without encountering a pediatric code blue. Or a physician might rarely see a case of malignant hyperthermia (a rare surgical emergency). Traditional training can discuss these in theory, but it’s hard to provide practical experience for rare events.
Traditional mannequins or classroom training can’t fully replicate the complexity or urgency of many real-world cases.
Low-Pressure Settings
Much of the current training occurs in settings removed from the hustle and urgency of actual patient care. Everyone knows in the scheduled skills lab that they are just going through a drill.
As a result, even if staff learn the steps of a procedure, they might not experience the stress that can affect decision-making.
Training Gaps for Interprofessional Communication
Another shortfall is that training often remains siloed by discipline and focuses on technical tasks. For example, doctors typically train on procedures, while staff members train on nursing tasks; however, they rarely train together.
While programs like TeamSTEPPS exist to promote teamwork, not all hospitals have implemented them thoroughly.
Making Patient Safety Training More Effective With VR
Here’s how VR is addressing the specific gaps in patient safety training:
Immersive Scenarios That Replicate Real Hospital Dynamics
VR can create richly detailed, realistic healthcare environments. Unlike a classroom lecture, VR surrounds the learner with the sights and sounds of a real clinical setting:
- The monitors beep
- Patients (in the form of virtual avatars) can cry or deteriorate
- Virtual attendants or coworkers are present
Modern healthcare VR simulations even incorporate physiologically accurate patient models. If a nurse pushes the wrong dose of a drug in the VR scenario, the patient avatar might show a drop in blood pressure or an arrhythmia.
Hands-On Decision-Making With Immediate Feedback
In a VR training module, the learner is an active participant, not a passive observer. They must make decisions and take actions as the scenario unfolds. Crucially, VR systems can provide instant feedback on those actions. For instance, in a VR infection control exercise, the program might visually highlight areas where contamination spread because the trainee missed a step.
Studies indicate VR learners feel far more confident in applying skills. One report noted a 275% increase in confidence to act on learned skills compared to those who only underwent e-learning.
Scalable, Repeatable Training Across Locations and Teams
Once a VR training module is created, it can be deployed to many learners and sites with minimal additional cost or logistics.
With VR, a hospital system can roll out the same training scenario to every clinical staff member across multiple campuses. Everyone just needs a headset (or even a standard computer, if the platform allows 2D access). Each VR patient safety training module can be repeated, adjusted, and scaled across teams.
VR also supports on-demand access. Staff can practice at convenient times without waiting for a scheduled class. For example, a nurse might conduct a VR refresher on handling patient falls during downtime on a night shift.
Benefits of VR-Based Patient Safety Training
Some of the key benefits of VR-based patient safety training include:
Higher Retention Rates vs. Traditional Methods
The immersive and interactive nature of VR helps learners retain more. That means they’re more likely to apply best practices instead of slipping back into old habits.
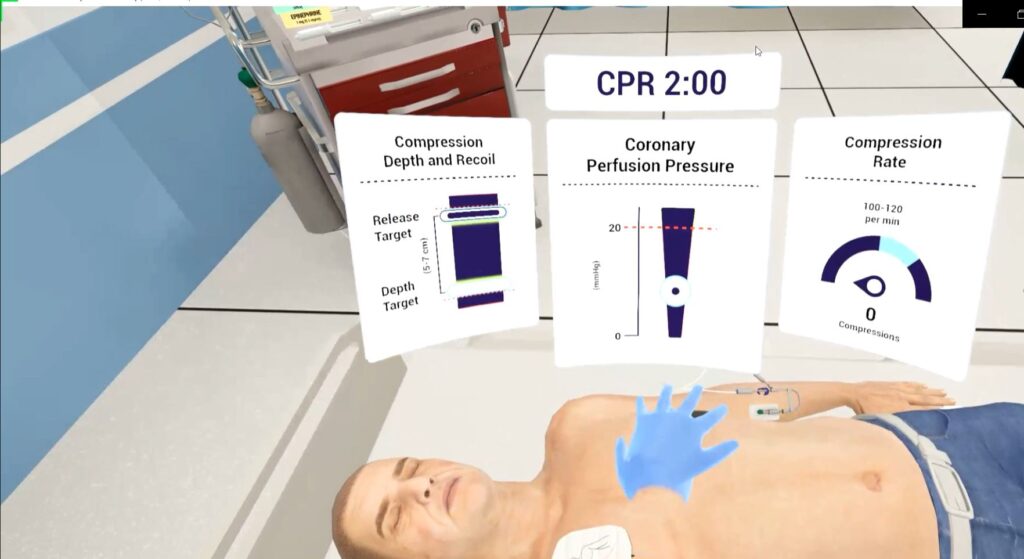
The active practice in VR also builds muscle memory. Take code blue resuscitation, for example. A clinician who has practiced them virtually dozens of times will remember the steps far better. That’s much more effective than just reading about the algorithm once or twice.
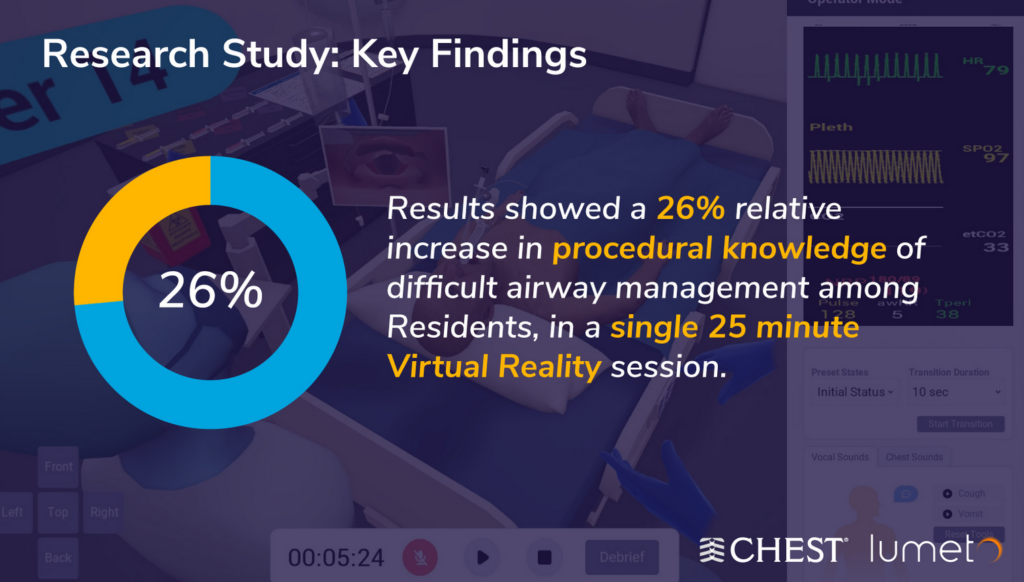
CHEST conducted scientific research studies across 3 leading academic institutions with the help of Lumeto. In the study, a single 25-minute VR session led to a 26% relative increase in procedural knowledge of difficult airway management among medical residents.
Safer Environment for Trial-and-Error Learning
Healthcare professionals can experiment and even fail in the virtual world without any risk to real patients. If a mistake is made (wrong dose, missed step, poor communication), it becomes a teachable moment rather than a cause for real harm.
Learners know they have essentially gotten a “second chance” many times over in VR. The scenarios can then be reset and tried again until mastered.
A participant in a VR training pilot noted the value of being able to “work out problems at their own pace” and practice during downtime, without interrupting patient care in the real world.
Real-Time Performance Tracking
VR training platforms have the built-in advantage of being software-based. With the power of artificial intelligence, they can automatically track a wealth of performance data.
For example, the system can capture:
- How long it took to recognize a critical change in vital signs
- Whether the user checked a patient’s ID band before giving medication
- How closely they followed the correct CPR steps
- Missed or delayed tasks during an emergency
- Time taken to complete each phase of a scenario
These metrics are presented on dashboards for both learners and instructors. Training leaders can demonstrate that 100% of staff completed key scenarios to a required proficiency level.
With Lumeto’s cloud-based trainer console, instructors can assess up to 5 users remotely in real time. Here’s an example:
Team-Based Learning
In multi-user VR scenarios, staff from different roles can enter the same virtual environment and communicate through headsets.
Even single-user VR modules often focus on communication. For instance, a learner might have to:
- Break difficult news to a virtual patient
- Address a disagreement with a virtual colleague
- Escalate care concerns using scripted dialogue branches
Studies on interprofessional simulation support that these experiences increase team effectiveness and prevent errors by creating challenging teamwork scenarios for practice.
Who Should Use VR for Patient Safety Training?
Essentially, anyone involved in training healthcare staff or managing patient safety initiatives should be considering how VR can enhance their programs. Key stakeholders who can benefit include:
Clinical Educators
With VR, a clinical educator can make sure every learner gets exposed to scenarios that are logistically hard to do in person (like a mass casualty incident or an ICU patient with multiple simultaneous issues).
Nurse Managers
Nurses can use VR training modules to routinely refresh their team’s skills without pulling everyone off the floor for in-service days. Because VR training can be done in short modules, managers could even incorporate it into nurses’ annual competencies or skills fairs.
The result for nurse managers is a more confident and prepared nursing staff. Some hospitals have reported that after VR training, nurses felt significantly more confident in handling emergencies in their unit.
Residency Program Directors
Residency directors could use VR to supplement in-person simulations, allowing residents to practice rare or critical cases virtually.
Program directors who adopt VR are likely to see trainees who are more uniformly competent and exam-ready. There’s also an attraction factor: modern learners often enjoy tech-based learning, so VR can enhance engagement and even be a selling point for a residency program’s innovation.
Risk Management Teams
Risk managers and QI specialists are always looking for ways to reduce errors and adverse events.
For example, incident reports may reveal a trend of errors in specific areas. For example, insulin administration mistakes or miscommunication during surgical handoffs might be common. In that case, the risk management team can develop a targeted VR training scenario to address the issue directly.
Infection Control and Compliance Officers
VR training is very well-suited for infection prevention education. Pilot programs have significantly improved compliance with hand hygiene and PPE use through immersive learning.
Because VR can visually demonstrate invisible threats (like the spread of germs), it can be more impactful than a lecture with slides of cartoon microbes.
Remote Healthcare Workers
Remote clinicians often miss out on in-person simulations. But they still face safety-critical decisions every day.
With VR, remote workers can:
- Train on the same scenarios as urban hospital teams
- Stay updated on protocols and emergency response
- Build confidence while working in isolated or low-resource environments
How Lumeto Helps Patient Safety Training Modules
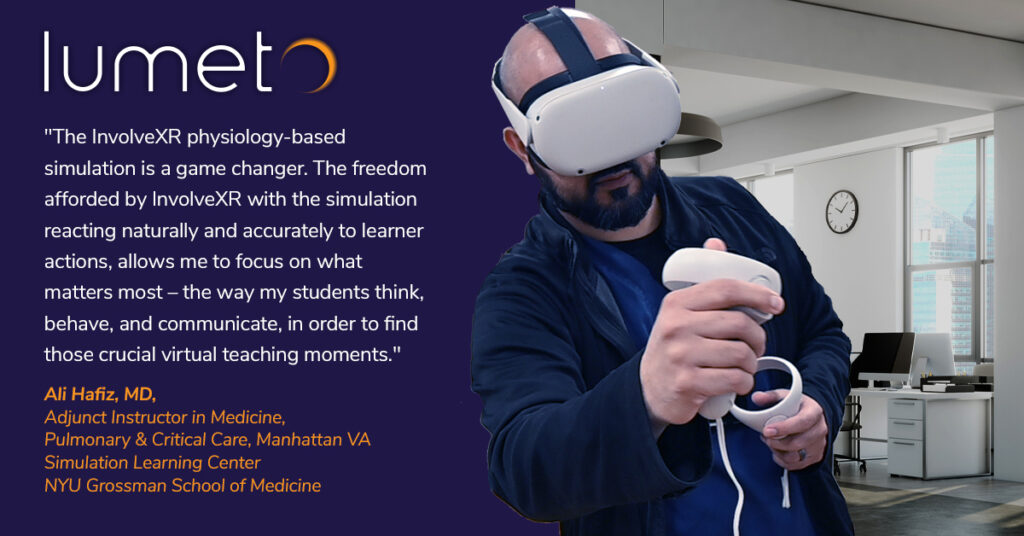
Lumeto is one of the leading companies providing VR training solutions specifically tailored for the healthcare industry. Our platform, InvolveXR, has features designed to address many of the needs we’ve discussed.
“I have been struck by how working with AI patients in Lumeto evokes an emotional response that mirrors interactions with human patients. The joy of making a breakthrough in patient communication or the sadness felt during a patient’s distress highlights the system’s realism and immersiveness. This emotional engagement makes each simulation a powerful tool for honing empathetic and professional skills as a nurse.”
— Kimberly Workum, University of Manitoba.
Here’s how Lumeto’s capabilities align with improving patient safety training modules:
Adaptive Learning Based on User Performance
Lumeto’s platform uses AI-driven techniques to adjust the training to each learner’s skill level. If a user is excelling, the system can introduce more complex challenges; if they’re struggling, it can provide guidance or simplify the scenario.
The idea is to avoid one-size-fits-all scenarios. Educational frameworks like Bloom’s Taxonomy are integrated to build from basic knowledge to advanced critical thinking progressively.
Role-Specific Training With Customization
Lumeto has modules tailored to the perspectives of various healthcare roles. For example, a nursing scenario might focus on bedside skills such as medication administration and patient communication. Whereas a physician scenario might involve diagnosis and decision-making in an acute situation.
Lumeto’s scenario library includes 100+ immersive learning experiences with 800+ customization tools. Trainees can improve their cultural competence by encountering diverse patient backgrounds (ages, ethnicities, comorbidities).
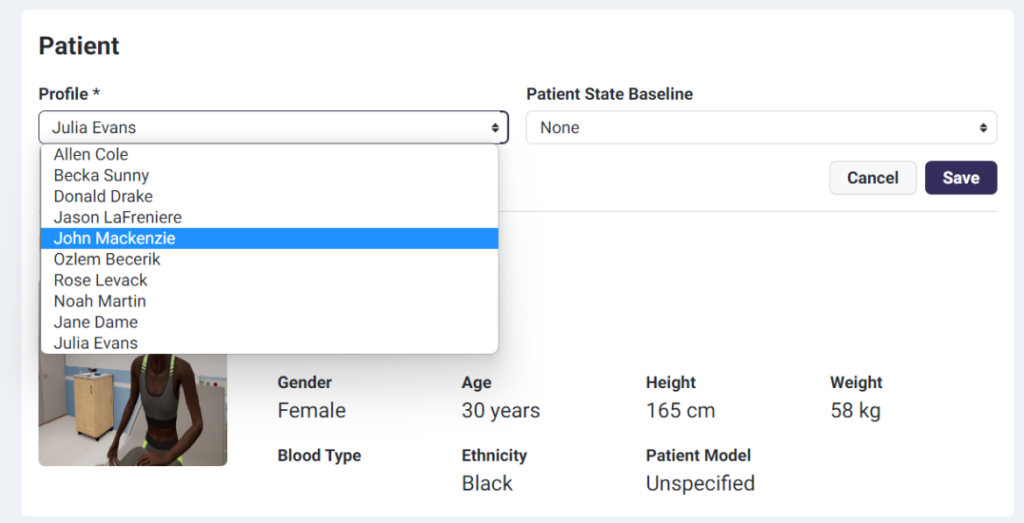
Trainers can also add/edit variables from training scenarios such as:
- Environment
- Medication
- Patient’s tests
- Assessment criteria
- Competency mapping and tracking
Here’s a look at Lumeto’s trainer’s app:

Remote deployment and accessibility
Lumeto’s platform works with consumer-grade VR headsets (like Meta Quest 2 or 3) and low-bandwidth networks. Even rural clinics or military medics can participate in training without needing expensive IT upgrades.
Accessibility also extends to timing, as it’s software-based. Staff can train on their own schedule (as long as they have the device and login).
Analytics Dashboards for Training Leaders
With Lumeto’s ACE (Artificial Clinical Evaluator), educators can automate and customize how they assess learners. Instead of relying on manual observation or generic scoring sheets, ACE maps competency performance to tailored criteria.
A training leader logging in can see metrics like:
- Completion rates
- Average scores
- Time taken to make decisions
- Frequency of critical errors
- Improvement over attempts
The top and bottom skills for each learner are identified. This way, training leaders truly drive quality improvement via education, armed with concrete data.

Give Your Team Real Practice With Lumeto
Every hospital wants training that feels real and works for everyone. But that’s tough to pull off. Simulation labs are great, but they’re hard to schedule and reach only a few people at a time. Slide decks and online modules are easy to roll out, but most people forget them by next week.
No one’s doing anything wrong. It’s just hard to create hands-on learning at scale, especially when time and budgets are tight.
Lumeto offers a way forward. Using VR, teams can step into high-stakes clinical situations (like code blues, ACLS, and BLS) and practice until they get it right. You get measurable results and consistent training that’s available anytime. See how Lumeto fits into your training program.
Frequently Asked Questions
How often should patient safety training be updated?
Patient safety training should be updated annually or whenever new guidelines, technologies, or safety concerns emerge.
Is patient safety training mandatory for all healthcare workers?
Yes. Most hospitals and healthcare systems require all clinical staff, including nurses, residents, physicians, and support staff, to complete patient safety training regularly. It’s often tied to accreditation standards and organizational safety goals.
What is the best way to measure the effectiveness of a patient safety training module?
Effectiveness can be measured through:
- Pre- and post-training assessments
- Competency checklists
- Incident or error rate trends
- Surveys that measure how confident learners feel after training
- Performance analytics
What is patient safety training for nurses?
Patient safety training for nurses teaches how to prevent harm during care. It includes protocols for medication safety, fall prevention, infection control, patient handoffs, and emergency response.