
Virtual Reality Doctor Training: From Classroom to Simulation
Doctors undergo some of the most rigorous and demanding training in any profession. But even the most detailed textbook/residency can’t fully replicate what happens when a life hangs in the balance.
Virtual reality doctor training is helping fill that gap. It adds a new, hands-on dimension to medical education without replacing traditional methods. With VR headsets, medical trainees can enter realistic clinical settings in a fully controlled environment.
A recent survey found that 77% of healthcare organizations have already adopted some sort of VR technology for medical training.
This article looks at how virtual reality is preparing future doctors for real-world challenges. We will also look at various applications, benefits, and challenges related to VR medical training.
What Is Virtual Reality Doctor Training?
Virtual reality doctor training uses computer-generated 3D environments to help medical students and professionals practice real procedures without risk. Instead of just observing, students are performing the actions themselves and seeing the consequences in real time.
Inside these simulations, doctors can perform everything from basic to advanced tasks, such as:
- Administering IV medications and calculating dosages correctly
- Managing a diabetic patient with sudden hypoglycemia in the ER
- Handling a hypertensive crisis or cardiac arrest in an emergency scenario
- Diagnosing abdominal pain linked to sepsis or pancreatitis
- Responding to critical cases like ectopic pregnancy or septic shock
- Performing a full head-to-toe patient assessment
A survey of healthcare-training organizations found 68.04% of respondents use VR to teach “hard skills” (e.g., equipment usage or new procedures).
Lumeto has been at the forefront of training doctors and nurses through AI-enabled virtual patients. Trainees can interact with simulated patients just as they would in real life.
The video below shows a medical provider managing a simulated stroke patient and assessing the symptoms using Lumeto’s platform.
Key Tools Used in Virtual Reality Training for Doctors
Modern VR medical training relies on a mix of software and hardware that work together to create realistic, responsive learning environments. Main tech includes:
- VR Headsets and Controllers: Headsets like the Meta Quest let doctors step into fully immersive 3D clinics. Hand controllers mimic medical tools, allowing precise actions such as holding a syringe or adjusting a ventilator.
- Haptic Feedback Devices: Some programs include haptic gloves or handheld devices that simulate the sensation of pressure, texture, or resistance.
- Simulation Software Platforms: Advanced software platforms such as Lumeto and similar systems power the actual virtual environments. These let instructors build clinical scenarios without coding.
- AI-Enabled Virtual Patients: AI technology adds realism by allowing virtual patients to talk, react, and show symptoms dynamically. Trainees can ask questions and listen to instant replies, just like in a real patient conversation.
- Performance Analytics Dashboards: Educators use built-in dashboards to review data (response times, decision accuracy, and procedural steps).

How Doctors Train with Virtual Reality (Step-by-Step)
VR training typically follows a structured session format. Below is a step-by-step look at how a doctor (or medical student) might train using virtual reality:
Step 1: Entering the Virtual Clinic or Operating Room
The trainee first puts on the VR headset (and any other gear, such as hand controllers or gloves). With modern platforms like Lumeto, often “only a headset and a laptop” are needed to launch a simulation.
The trainee typically receives a briefing on the scenario either via on-screen instructions or by a narrator.
Once the scenario is launched, the user finds themselves inside a virtual medical setting. It could be a fully equipped operating room with a patient on the table, or an emergency medical camp on a military site. The trainee can look around 360° to see the patient, medical equipment, monitors, and even virtual colleagues in the room.
Environmental elements such as lighting, sound, and even simulated background chatter or alarms may be present to make it feel authentic.
Here’s a trainer introducing a ventilator to medical students in a VR simulation:
Step 2: Performing Simulated Procedures Safely
Once inside the scenario, the trainee proceeds to examine and treat the virtual patient as they would in real life.
During the VR scenario, the virtual patient provides realistic feedback to the trainee’s actions. For instance, if the doctor in training intubates the patient’s airway correctly, the oxygen levels on the virtual monitor will improve. If they choose an incorrect drug, the patient’s blood pressure might crash (simulating a bad reaction). The trainee learns from the mistake in a consequence-free environment.
Many VR medical training platforms allow multi-user participation in the same virtual scenario. Several clinicians (possibly in different physical locations) could collaboratively manage a VR case together.
Here’s a real example from Lumeto’s VR platform where a student accidentally administers the wrong dose to a virtual patient. But their teammate quickly identifies the error and takes corrective action:
Step 3: Receiving Instant Feedback and Performance Metrics
One of the powerful features of VR training is the ability to receive immediate performance feedback. As soon as the scenario ends (or even during it), the system can present performance metrics: for example,
- The time taken to complete the procedure
- Whether critical steps were done in the correct order
- How the virtual patient’s vital signs changed, and so on.
Some VR training programs also have a “tutor mode” or AI instructor that will flag errors in real-time.
After the session, there is typically a debriefing. This could be done by the software and/or by a human instructor.
VR platforms like Lumeto generate a summary or even a replay of the trainee’s performance. Educators or the trainees themselves can review this replay to discuss what went well or what could be improved.
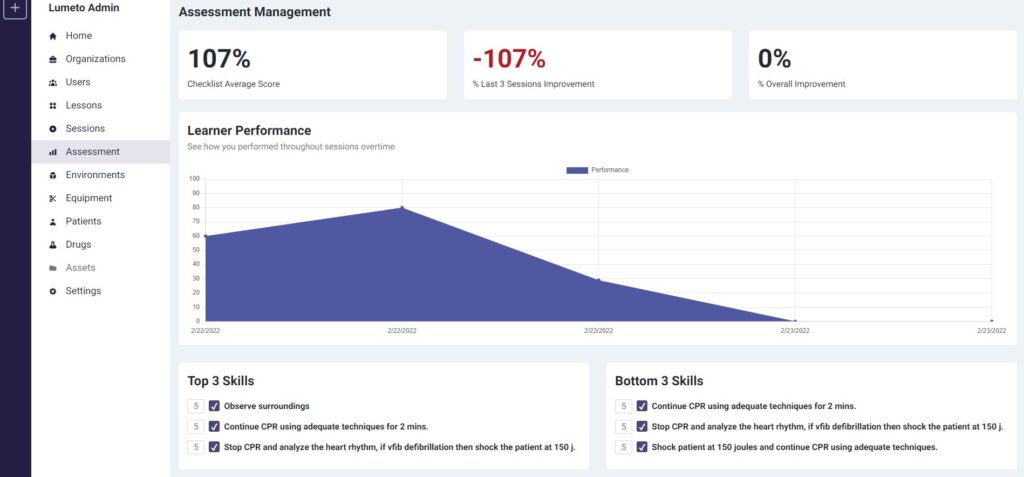
An instructor can also review the saved performance data or video after, and then provide targeted coaching.
Benefits of Virtual Reality for Training Doctors
Virtual Reality offers numerous benefits for medical training, which is why it’s gaining traction in healthcare education. Below are some of the key advantages, each addressing a pain point of traditional training:
Safe Practice Without Risking Patient Safety
The World Health Organization (WHO) reports that 1 in every 10 patients is harmed while receiving care, and over half of those cases are preventable. Medication errors alone account for nearly 50% of this avoidable harm.
The financial toll of medication-related harm in the U.S. is significant, with morbidity and mortality costs estimated at around $77 billion per year.
Virtual reality helps reduce those risks by allowing students to practice procedures in a completely safe, simulated environment. They can make mistakes, learn from them, and try again without endangering real patients.
Realistic Exposure to Rare Cases
A survey of medical students in the U.S. & Canada found that 92% of respondents felt ill-prepared to provide care for patients with rare diseases.
VR can compress decades’ worth of rare case exposure into a short training period. A medical student could experience ten different rare crises in a single afternoon of VR training—something that could take many years of clinical practice (or pure luck) to encounter otherwise.
Team Collaboration
It’s not always feasible to assemble a full team and a patient simulator mannequin for frequent drills. But with VR, each member can participate by just putting on a headset, even from different rooms.
VR simulations include roles for doctors, nurses, and paramedics, allowing everyone to train together in real-time. Training together breaks down silos and teaches everyone to understand each other’s roles.
In one example, NYU students using Lumeto’s VR platform practiced Advanced Cardiac Life Support (ACLS) together. Each team member performed their assigned role:
- Administering chest compressions
- Preparing medication
- Managing airways
Here’s a video below:
Enhanced Emotional Intelligence
VR enhances empathy by allowing providers to experience the patient’s perspective literally. Doctors can learn essentially the “soft skills” of healthcare, such as:
- Bedside manner
- Stress management
- Active listening
- Cultural competence
- Effective doctor-patient communication
Studies show that VR learners feel 3.75 times more emotionally connected to the material than those learning in a traditional classroom.
Lumeto’s platform takes this further with AI-powered virtual patients that respond in real time. For example, a student must calm an angry patient who’s frustrated about a delayed diagnosis. The AI patient reacts naturally (crossing arms, changing tone, or showing visible agitation) in response to the learner’s choice of words and tone.
Eco-Friendly and Resource-Efficient
In VR, all the tools and supplies are virtual. It doesn’t pose biological hazards (e.g., risk of spreading infections or blood exposure), unlike real clinical training.
You can practice a surgical procedure 100 times in VR without using a single actual scalpel blade, suture kit, or piece of gauze. Once the software is created, repeating scenarios have no recurring consumable cost.
Running a VR training program consumes some electricity (for computers and headsets). But it has a much smaller footprint than a full simulation center (requiring multiple rooms, heavy manikins, lighting, etc.) and might be used only intermittently.
With VR, neither trainees nor instructors need to travel to a single location. This can reduce the carbon footprint of training events (no flights or long drives required for a VR session).
On-Demand Training Access
Traditional medical training often depends on scheduling. You have to wait for an available instructor or a particular patient case to come along. VR breaks those constraints by providing on-demand training.
On-demand access also means more practice opportunities. Trainees can revisit VR scenarios days or weeks later as refreshers.
Virtual Reality Medical Training vs. Traditional Training
It’s worth comparing VR-based training head-to-head with traditional medical training methods to understand their differences, advantages, and limitations.
Realism and Repetition
VR training offers a high degree of situational realism through visuals and scenarios. Trainees can walk into a virtual operating room, check monitors, and perform complete procedures step by step.
However, current systems still have limits. Most VR programs don’t yet fully replicate the sense of touch (e.g., the texture of an organ). Traditional methods, like practicing on cadavers or during live surgeries, still provide that essential tactile feedback.
Developers are closing this gap with haptic technology, including gloves and handheld devices that simulate pressure or resistance. It allows learners to “feel” when they apply too much force or make the proper incision depth.
At Children’s Hospital Los Angeles (CHLA), first-year resident Travus White, MD, described the experience vividly: “You can’t get that same rush from a written exam,” he said. “You feel it when you’re inside the scenario, and this is about as close to real life as it gets.”
Todd Chang, MD, CHLA’s director of research and scholarship, added that the immersion is measurable. When students engage fully in his VR simulations, their heart rates rise by about 10%.
Training Time
When it comes to efficiency and time, VR training can potentially accelerate learning in some areas compared to traditional training.
Traditional training often has a lot of downtime or waiting. In contrast, VR training is very focused on time-on-task. Trainees can also replay their own training sessions to review mistakes or observe how they performed under pressure.
Some programs, like Lumeto, even allow students to watch others train live through shared screens, turning each session into a group learning opportunity.
VR can reduce the time to initial competency (the first phase of learning) by providing intense practice, but it shouldn’t eliminate the slower accumulation of wisdom that comes from real-life exposure.
For faculty, VR saves time as well. Traditional training often requires a supervising doctor for every practice (e.g., an attending surgeon scrubbed in with a resident). VR can allow a trainee to practice some things independently, freeing up faculty time.
Trainer’s Feedback
In traditional medical training, feedback comes directly from experienced mentors. An attending physician might observe a trainee in the clinic and later discuss what went well, or what didn’t. This kind of feedback is rich, personal, and rooted in clinical experience. But it can also vary between instructors and often arrives after the fact.
Many VR training systems provide instant, data-driven feedback, showing metrics, alerts, or scores in real time. Trainees can immediately see when they’ve made an error or when their technique improves. While VR feedback is often more objective, it can lack the depth and nuance of human insight.
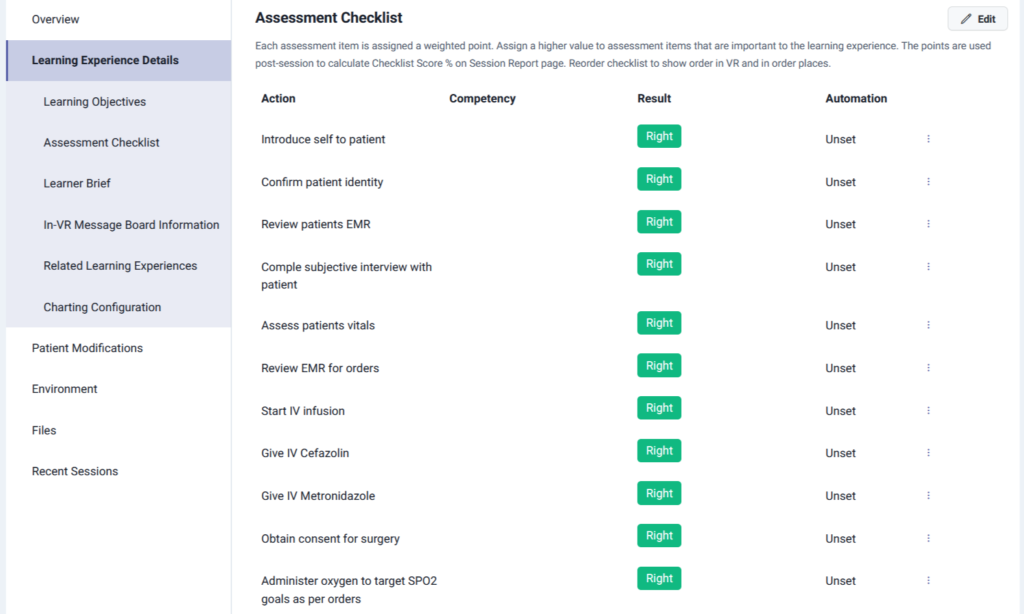
Here’s a look at how Lumeto’s VR training platform automatically evaluates learner performance through a detailed assessment checklist:
Ethical Concerns
Virtual reality also helps resolve several long-standing ethical and practical issues in medical training. Instead of practicing on real bodies or live patients, trainees can build competence safely in a virtual environment.
Here’s how VR addresses common ethical challenges:
- Cadaver training: Students can practice dissection or surgical techniques without relying on human donors, addressing issues of limited availability, cultural sensitivities, and consent.
- Animal testing: VR provides an alternative to using live animals for procedural training, eliminating ethical concerns about animal welfare while still teaching anatomy and technique.
- Supervised patient encounters: Trainees can learn communication, diagnosis, and treatment planning without putting patients at risk of discomfort, misdiagnosis, or unnecessary exposure.
See How Lumeto Trains Better, Confident Doctors
Lumeto’s InvolveXR gives healthcare professionals the tools to train smarter and faster. Hospitals and universities use Lumeto to accelerate readiness among doctors and strengthen clinical decision-making from day one. Here are some key highlights of Lumeto’s VR training platform:
- 100+ Immersive Learning Experiences: Access a vast catalog of real-world medical scenarios across emergency, surgical, and clinical care.
- Create Your Own Virtual Patient: Use generative AI to design lifelike patient cases that adapt to decisions in real time.
- Multiple Languages: Train teams globally with localized modules and voice interactions in several languages.
- Dedicated Ongoing Support: Get continuous technical and instructional support to ensure smooth implementation and measurable results.
FAQs About Virtual Reality Doctor Training
Is virtual reality doctor training expensive to implement?
Costs vary depending on the size of the program and equipment needs. Many VR platforms work on standalone headsets like Meta Quest. This makes them more affordable than traditional simulation centers that require physical mannequins and dedicated rooms.
What kind of cases can be practiced in VR?
Trainees can handle everything from routine patient assessments to complex emergencies such as cardiac arrest, diabetic ketoacidosis, or septic shock.
Are VR simulations customizable for different hospitals or specialties?
Institutions and healthcare trainers can create custom scenarios based on their training protocols. VR platforms allow users to design or modify virtual patients, set conditions, and adjust difficulty levels without coding.
What medical specialties use VR the most?
VR training is widely used in nursing, emergency medicine, anesthesiology, internal medicine, and pediatric training. It’s also expanding rapidly in mental health, obstetrics, and rehabilitation therapy.
What challenges do hospitals face when adopting VR training?
Initial setup costs, faculty training, and integration with existing curricula are common challenges. However, most institutions find that they are outweighed by long-term benefits like reduced resource use and scalable training access.